LESSONS FROM FIGHTING THE COVID-19 PANDEMIC
Recent covid crises exposed the lack of connection between governmental discourses as well as the promotion of OH in International contexts and the lack of surveillance systems, which would be both comprehensive and efficient. To this day, the COVID-19 pandemic still has heavy consequences in many areas worldwide. Yet, its emergence remains a mystery. The surveillance and prevention system has failed in many regards, such as biological surveillance in animal reservoirs, identification of facilitators of emergence as well as transmitters, and actions taken for disease control. Surveillance being the key to prevention and control, the response should have brought data on three factors, namely virus emergence surveillance, factors of transmission and early detection of human infections.
Being most likely a zoonosis, like previous coronaviruses, the COVID-19 is a One Health issue by excellence. It demonstrates Interdependence of human, animal and environmental factors. Yet, healthcare systems worldwide proved not to be ready yet to face such threats, being solely focused on human health. During this last crisis, the lack of waring system and of collaboration between stakeholders at an early stage dit not enable an efficient enough response. The lack of multisectoral cooperation hindered the sharing of information about the new virus, its spreading and is adaptation mechanisms. For instance, zoonoses present risks of reverse transmission between humans and animals, and the Omicron variant was very likely a result of this phenomenon. Mutations are to be expected, and the evolutionary process should have been better anticipated taking these risks into account.
Overall, scientists agree on the urgency of going beyond what has already been done in terms of One Health so far. Despite an increasing amount of research and political acknowledgement, One Health structures and projects remain poorly funded, and still too theoretical. During the last crisis, cooperation at both local and global levels was not sufficient to enable an adequate response.
A NEW FRAMEWORK FOR ACTION AT EACH STEP OF A PANDEMIC CRISIS
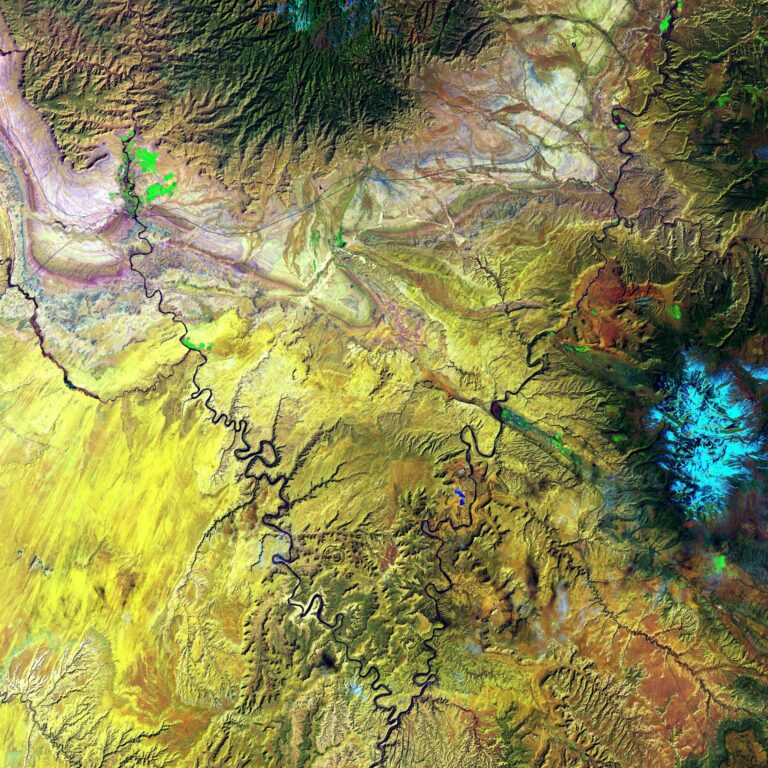
According to the authors, a more targeted health prevention system is needed, and socioecological systems must evolve towards a more resilient path. First and foremost, prevention, preparedness and early detection should become the basis of all action. The contributors indeed suggest that common lists of pathogens monitored by public health actors be published, and constantly kept up-to-date, and reinforced in case of of the rise of a new pathogen. This action requires the development of common indicators and the generalization of interdisciplinary data sharing. Moreover, international cooperation should be pushed further, to develop a common worldwide health vision. The authors recommend the creation of a list of hotspots, as well as long-term programs funded by multiple mechanisms and including the World Bank.
In order to be effective, the new health systems should become universal and radically intersectional. Firstly, there is a real need for a new global comprehensive vision taking into account ambitious initiatives at all levels. The One Health reform should indeed be carried by newly-created inter-ministerial platforms in all countries, while cooperation between local and supranational entities is being reinforced. Secondly, predefined One Health structures designed to lead crisis management and using all abilities, should be given a central role. These should be multidisciplinary and consider multiple factors, (environmental, social, economic, ethical, political). To enable a rapid decision-making process, the authors stress the importance of including insights from social science into the fight against pandemics, as well as artificial intelligence.
Finally, the mobilisation of the civil society appears to be of the utmost importance. The recommended reforms indeed consist in strong restructurations of healthcare systems in all countries, which would result from bottom-up restructuration. The authors of the article recommend that One Health education and training be provided for all health and environmental-related professions, entailing the creation of common curriculum in schools, to enable the development of much-needed cross-curricular skills among professionals.
SOURCE
After 2 years of the COVID-19 pandemic, translating One Health into action is urgent.
By Prof. Denis Malvy, MD, Prof Laetitia Atlani-Duault, PhD, Prof Daniel Benamouzig, PhD, Prof Pierre-Louis Druais, MD, Prof Yazdan Yazdanpanah, MD, Prof Jean-François Delfraissy, MD, Prof Bruno Lina, MD.
DOI: https://doi.org/10.1016/S0140-6736(22)01840-2
Published on October 24, 2022